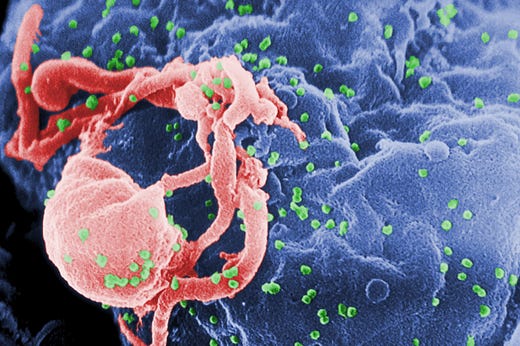
The evidence is clear: there are substantial similarities between SARS-CoV-2 and HIV-1!
The currently available COVID-19 vaccines must be put to a halt NOW and investigations need to commence as we speak!
The following represents a set of extracts from my recent scientific preprint, highlighting the peculiar similarities between SARS-CoV-2 and HIV-1, as well as between systemic COVID-19 and AIDS.
“With regards to the origins of the virus, the scientific community is now divided into two major groups. The first group believes it fully underwent natural selection and that the first infection incident that was related to the Huanan sea market occurred after a zoonotic process took place between bats and humans, via the pangolin species. The second group believes that, as the virus was being naturally selected and undergoing a process of zoonosis, local laboratory researchers isolated the evolving virus in the P4 section of Wuhan’s Institute of Laboratory and added to it further antigens in order to test the reaction of the immune system in certain bats. As time went by, more and more evidence that the virus underwent a “gain-of-function” research before an accidental or a deliberate lab-leak occurred was presented in scientific literature. Moreover, there are peculiar commonalities between the novel coronavirus and the human immunodeficiency virus at genomic and morbidity levels. It may be suspected that SARS-CoV-2 underwent a distant form of co-evolution with HIV-1, given the existence of similarities between SARS-CoV and HIV-1, and that an alleged gain-of-function research of the coronavirus increased the speed of a possible process of molecular “alikening” with the retrovirus in cause. It may also be suspected that genomic evidence with regards to such a matter remains substantial, despite the retraction of a preprint showing genomic similarities, given the lack of author’s reasonable explanation for paper retraction, as well as the existence of a molecular mechanism called LINE-1/HIV-1 Reverse Transcription, which was shown in a number of clinical occasions to insert around 1% of the viral genome - including approximately 1% of the +ssRNA encoding the spike protein - into the DNA of the host cell. It is far less common for other natural RNA viruses that are not retroviral in nature to experience reverse transcription in the human body, and there is virtually no scientific literature covering such an event for other non-retroviral RNA pathogens. Interestingly, there was a widespread antiretroviral drug repurposing for COVID-19, which included the Highly Active Antiretroviral Therapy (HAART) for gut-related virus-induced pathogenesis, as well as ritonavir, lopinavir, darunavir and nelfinavir(Yu et al., 2021). Moreover, both ssRNA viruses implicate the AIP4 protein as an important target for virulence, significantly affecting the quality of the induced interferon system’s activity (Olga Tarasova et al., 2020), and neuropilin-1 (NRP1) and the human Vascular Endothelial Growth Factor Receptor 2 (hVEGFR2) also represent important molecular and therapeutic targets for both SARS-CoV-2-induced COVID-19 and HIV-induced AIDS (Abel et al, 2022). The CXCR4 (Lourda M. et al, 2021) and CCR5 (Agresti N. et al., 2021) receptors on the helper CD4+ and cytotoxic CD8+ T-Lymphocytes were also shown to be significantly dysregulated following a SARS-CoV-2 infection of CD4+ helper and CD8+ cytotoxic T-lymphocytes, and CXCR4 (Daoud et al., 2022) and CCR5 (Patterson B. K. et al., 2021) receptor inhibitors have displayed a substantial level of efficacy against COVID-19 and AIDS. Both viruses may directly dysregulate important T-lymphocyte activities and often cause significant morbidity in the gastrointestinal tract. As a result, SARS-CoV-2 is likely also capable of infecting CD4+ and CD8+ T-lymphocytes, and of substantially dysregulating the activities of the CXCR4 and CCR5 receptors on their cellular surface (Agresti N. et al., 2021). The virus was also shown to be the most virulent in the circulatory system, and not in the respiratory system, and mucosal immunity was shown to be the strongest restricting factor for viral infectious spread in the body. It may be that a SARS-CoV-2 co-evolution with HIV-1 would have a major impact upon the safety and effectiveness of the spike protein-based vaccines, and there may now be substantial reasons to believe that the ongoing mass vaccination should be halted and re-evaluated, given the approximately 1 in 800 recently projected ratio of severe adverse event per administered vaccines, and the evident immune evasion of new viral variants, despite the multiple number of administered vaccine doses. […]
The SARS-CoV-2 genome translates the spike glycoprotein, which is the principal viral component inducing pathogenesis in humans. The open reading frame of the viral genome translates 16 non-structural proteins, as well as certain open reading frame products, which are implicated in the delay and temporal reduction of first-line immune-stimulatory signaling. The virus also aids the formation of reactive oxygen species and produces tunneling nanotubes (TNTs) in the cytoplasm of host cells by means of evading recognition by Pattern Recognition Receptor and preventing the expression of genes encoding Type I and Type III Interferons (Rubio-Casillas A. et al., 2022). Although such a viral mechanism plays a secondary, passive role in sustaining infection and facilitating a steep rise of the viral load in the body, it actually plays a bigger part in the development of life-altering and life-threatening pathology in many patients. Similar events occur during Influenza A, which explains why clinicians developed a vaccine using a live-attenuated Influenza A viral copy that has a loss-of-function kind of mutation induced in a region of the open reading frame that encodes non-structural protein 1 (NSP1). Although such an approach could be the best attempt to immunize the human body against Influenza long-term, the cells are still not very directly trained to produce Type I and III Interferons more robustly and outcompete the evolutionary ability of the virus to silence the interferon system via the translation of non-structural proteins as such.
Acquired Immunodeficiency Syndrome, which is in short known as AIDS, represents an immunological disease caused by an HIV infection, and it involves layers of human genetics, immunology and infectious diseases. A number of people do not experience disease at all and survive until they experience death as a result of elderly age, whilst other people eventually develop progressively harsher disease, which eventually results in their death. Immunogenetics plays a major role in the determination of disease progression and prognosis in each person, and such a phenomenon determined health authorities to recommend protection during sexual intercourse, as well as an asymptomatic method of testing to detect a presence or absence of a viral load in the human body. The disease is widely transmitted sexually and many people have become infected due to unprotected sexual intercourse. In the 1980s, there were significant controversies with regards to the approaches of therapy development and rollout, and many people suspected that inexpensive, first-line immunomodulatory approaches had not been prioritized to attempt a prevention of the onset of the disease in many. Dr. Anthony Fauci was situated in the central area of suspicion that expensive, corporation-oriented approaches were prioritized. From the beginning of the HIV-induced AIDS pandemic, Dr. Anthony Fauci recognized the efficacy of low-dose Type I Interferon-based substances as a potential vaccine against AIDS, but for a less recognized reason, such products did not undergo significant and widespread clinical testing, despite their life-saving effects.
It has been suggested that SARS-CoV-2 and HIV-1 have similar evolutionary patterns, and mutations of both ribonucleic acid-based viruses led to substantial escape from previously-developed antibodies and increase of infectivity, which is accompanied by an increase of virulence (Fischer et al., 2021). Both SARS-CoV-2 and HIV-1 infections result in impaired Type I and III Interferon signaling and induced signaling cascades, as well as in a pronounced impairment of T-lymphocyte activation. Both viruses target the AIP4, NRP-1 and hVEGFR2 proteins, which are implicated in regulatory processes against hyper-inflammatory responses, in the fortification of the endothelial barrier and prevention of metastasis respectively. Both viruses also bring significant disruptions to the expression rates of the CXCR4 and CCR5 receptors on the surface of CD4+ helper and CD8+ cytotoxic T-lymphocytes. The CCR5 receptor was shown to be important therapeutic target for the diseases induced by both SARS-CoV-2 and HIV (Agresti N. et al., 2021), whilst the expression rate of the CXCR4 receptor was found to be affected following SARS-CoV-2 infection (Lourda M. et al., 2021), and the latter receptor was also targeted during a Positron-Electron Tomography (PET) kind of molecular imaging for the investigation of a severe form of COVID-19 (Lambertini A. et al., 2022). Leronlimab, Maraviroc and inhibitors of Protein Tyrosine Phosphatase 1B (PTP1B) represent three therapeutic agents that substantially regulate the activities of the CXCR4 and CCR5 receptors on important types of T-lymphocytes in patients with COVID-19 and AIDS. Clinicians discovered that around 1% of the SARS-CoV-2’s genome, as well as around 1% of the spike protein-encoding +ssRNA, is reverse transcribed and integrated into diverse important human cell lines, such as hepatocytes, and such a molecular phenomenon is extremely uncommon during infection by other ribonucleic acid-based viruses. Not to mention that such an event can lead to increased risks of mutation, tumor formation and genome toxicity, particularly if the viral load or any genetic viral fragments reach major sanguine and lymphatic vessels. Moreover, therapeutic approaches that have been widely used to treat moderate and severe stages of COVID-19 are also widely used to treat important stages of HIV-1 infection. Importantly, the pathogenesis of COVID-19 is often followed by the development of autoimmunity and even of a commencement of an immune decay, particularly in people with one or more significant comorbidities. Recently, Germany’s Health Minister warned that SARS-CoV-2 infection is rather often followed by a transient T- and B-lymphocyte-related immunodeficiency (i.e. lymphopenia), and an ACE2-independent infection of important lymphocytes might explain such a phenomenon, which is likely more prevalent when the viral load has reached a systemic level in the human body. Earlier, the director of the Intensive Care Unit of the Zhongnan Hospital of the University of Wuhan, Peng Zhiyong, stated that the COVID-19 effects upon the human organism were like a combination of COVID-19 and AIDS, as the disease would damage both the lower respiratory tract and the immune system. It is important not to forget that the Nobel Prize Laureate for the discovery of the human immunodeficiency virus (HIV), Dr. Luc Montagnier, stated his concerns with regards to possible insertions of HIV regions into the SARS-CoV-2 genome prior to a laboratory leak, and that people particularly receiving at least a third dose of the currently-available COVID-19 vaccines would be at a significantly increased risk of experiencing AIDS-like negative impacts upon their immune system.
It is important to note that a set of similarities represents a spectrum, rather than a yes-or-no question with regards to whether two microbes are genetically identical. And such a spectrum applies differently, depending on the context and background of the two genetic toxins to be compared. With regards to a genetic and phenotypic comparison between SARS-CoV-2 and HIV-1, it is important to apprehend that even a pronouncedly small degree of similarity could impact scientific and research perspective if such a level of similarity affects important areas in therapeutics and vaccinology, for example. Even if the two single-stranded ribonucleic acid-based viral agents are widely different from each other, if there is a genetic similarity in a few ribonucleic acid areas that are part of the viral genome impacting human immunity directly, then it is rather likely that the latter viral agent would also affect human immunity in similar patterns, which would affect the general approach of therapy and vaccine-development. Likewise, specific similarities between SARS-CoV-2 and HIV-1 with regards to induced immunopathogenesis does not ultimately indicate the coronavirus contains direct inserts from the retrovirus in cause, just as small-scale genetic and evolutionary similarities between the two viruses does not ultimately indicate a laboratory origin. In medical and biomedical research, it is likely crucial to hold fast to having an open mind and a humble approach in order not to become victims to the elementary, and yet still tricky, fallacy of “it is sunny, therefore it is not raining”. It is therefore a likelihood that the mechanisms and genetic origins of the novel coronavirus deserve further investigations to address found similarities in immunopathogenesis, genetics and proteomics that may be of significant concern, and to clarify genuine questions that numerous members of the public may be having, given that not every citizen and resident of the world has a degree in medicine or a biomedical science-related domain and that not all questions are in accordance with far-fetched conspiracy theories.
Methods
An extensive search in major academic databases, including PubMed, EuropePMC and ResearchGate, was conducted using keywords, such as SARS-CoV-2, COVID-19, HIV-1, HIV-1 Reverse Transcription, viral co-evolution, first-line immunity, COVID-19 vaccine adverse events and lymphopenia. For the PubMed database, the [MeSH] conducting algorithm was used to find scientific literature of particular concern. Genetic, protein-related and morbidity-related searches were performed, given that evolutionary similarities at the genome level may project the similarity to levels of proteomics and disease manifestation. The standard scientific literature review procedures have been aimed for in this paper and we highlighted results collected using computational biology methods suggesting that there is a direct correlation between four fragments of the spike glycoprotein and certain regions from the gp120 and gag glycoproteins that are found in the HIV genome. Namely, the GTNGTKR, YYHKNNKS, G0SSSG and QTNSPRRA amino acid sequence inserts in the SARS-CoV-2 spike glycoprotein had not been found in previous coronaviruses and they had been determined to be genetically similar with specific regions of the gp120 and gag retroviral proteins (Pradhan et al., 2020). The computational biology methods used to compare the concerned structures were evaluated with care and using an objective approach.
Results
Following a rigorous procedure of literature search and review, similarities of significance were found on genomic, proteomic, disease-manifesting and pharmacological levels. A significant extent of scientific literature concerning HIV-1 Reverse Transcription was found in the case of COVID-19 infection and virtually no literature concerning the same HIV-1 Reverse Transcription phenomenon following infection by other RNA viruses was found. There is a much wider extent of immunological adverse reactions caused by the novel COVID-19 vaccines than the flu vaccines, with a number of symptoms that show a degree of similarity with AIDS symptoms, although the extent of such a symptomatology has been shown to be more restricted. Although one preprint paper concerning similarities between four unique inserts in the SARS-CoV-2 spike glycoprotein and the HIV gp120 and gag proteins was retracted, there was no reasonable explanation of the authors for their decision, and scientists who attempted to dispute such a study tended to be more negational in their approach, and less factual. There was no found evidence to suggest that there is minuscule or no commonalities between the two viruses, which would far more likely be a result of a zoonotic viral transmission leading to a consequential disease outbreak in humans. On the contrary, many results suggested the existence of significant similarities between the two ribonucleic viral agents; similarities that may deserve a general investigation involving a genetic comparison between them. For example, the gp120 is known to interact with the CCR5 receptor on CD4+ and CD8+ T-lymphocytes (Guryanov et al., 2019), and SARS-CoV-2 is known to infect such CD4+ and CD8+ T-lymphocytes and substantially dysregulate the activity of their CXCR4 and CCR5 receptors (Agresti N. et al., 2021). […]
Discussion
There are peculiar common characteristics of both COVID-19 and AIDS molecular pathology and therapeutics. Namely, both SARS-CoV-2 and HIV-1 interact with the AIP4 inflammatory protein, and both molecular interactions were found to lead to an inhibited first-line immunity. Both ssRNA viruses decrease the expression and signaling rates of interferon-alpha/beta, -epsilon and -lambda, as well as the polarization of the Th17 lymphocytes (DaFonseca et al., 2015). Immunocompromised people were found to be more prone to the development of molecular pathophysiologies, such as a cytokine depletion and the onset of hemophagocytic lymphohistiocytosis, which is in short known as cytokine storm, following an infection with both SARS-CoV-2 and HIV-1 (Olga Tarasova et al., 2020). Moreover, the human Vascular Endothelial Receptor 2 Growth Factor Receptor (hVEGFR2) was found to be a significant target for both viral infection and therapeutic agents in the case of infection with both SARS-CoV-2 and HIV-1 (Abel et al., 2022), as both viruses target neuropilin-1 (NRP-1), reducing its expression rate and leading to a lower quality of the endothelial barrier’s function, as well as to a dysregulated T-lymphocyte activity (Naidoo et al., 2022). Also, it was determined that SARS-CoV and SARS-CoV-2 may exhibit a direct activity of T-cell activity inhibition, as the human immunodeficiency virus 1 also does (Sigalov A.B. et al., 2022), and the novel coronavirus often infects T-lymphocytes without the activation of the Angiotensin-Convertase Enzyme 2 (ACE2) receptor (Xu-Rui Shen et al., 2022). It is known that hVEGFR2 represents a major target for tumor cells to undergo the process of metastasis in cancer. Given that an HIV-1 infection is rather significantly associated with an increased incidence of malignant tumor formation and consequently, with metastasis, it is possible that the evolutionary process that led to the selection of SARS-CoV-2 may have made the novel virus more similar to HIV-1. Furthermore, there was a widespread repurposing of antiretroviral drugs, which are mainly HIV protease inhibitors, for COVID-19 from the beginning of the pandemic. Antiretroviral drug-like compounds, such as ritonavir, lopinavir, darunavir and nelfinavir (Yu et al., 2021) were widely repurposed for the treatment of COVID-19 in the ICU departments of major hospitals worldwide. The effects of the repurposed drugs were controversial for a significant number of hospital patients (Agarwal et al., 2020). The Highly Active Antiretroviral Therapy (HAART) is a significantly effective treatment against major forms of intestinal damage following HIV infection, which indicates another commonality between SARS-CoV-2 and HIV-1 infection; significant damages of the gastro-intestinal tract (GI) (Costiniuk C.T. et al., 2012). Most importantly, molecular therapies implicating the disruption of CXCR4 (Daoud et al., 2022) and CCR5 (Patterson B. K. et al., 2021) CD4+ T-helper and CD8+ cytotoxic T-lymphocyte receptors have led to significant improvements in the prognosis of the disease for both SARS-CoV-2-induced COVID-19 and HIV-induced AIDS (Agresti N. et al., 2021), the +ssRNA viral genome was found to dysregulate the expression rate of the CXCR4 receptor as well (Lourda M. et al., 2021), and the CXCR4 receptor was also targeted by Positron-Electron Tomography during molecular imaging in a severe form of COVID-19 (Lambertini A. et al, 2022). One significantly effective therapeutic agent that inhibits both CXCR4 (Elneil et al., 2021) and CCR5 (Agresti N. et al., 2021) receptors, in patients with COVID-19 and AIDS, is the Leronlimab immunoglobulin. A therapeutic agent that inhibits the CCR5 receptor and significantly improves the health state of COVID-19 and AIDS patients is Maraviroc (G. M. Basha et al., 2021). Inhibitors of protein tyrosine phosphatase 1B (PTP1B) were found to inhibit the aberrant activity of CXCR4 receptors in patients with severe COVID-19, improving their prognosis (Song et al., 2022), and statins were also found to reverse the disrupted activity rates of important T-lymphocytes in patients suffering either from COVID-19 (Di Simone et al, 2021) or AIDS (Nabatov A. A. et al., 2007). In AIDS patients, statins were specifically found to regulate the activity of the affected CXCR4 and CCR5 receptors on the surface of CD4+ and CD8+ T-lymphocytes (Higuita et al., 2013), meaning that it is likely that they have the same receptor-specific therapeutic effects in patients with severe COVID-19. Interestingly, cyclic treatment-interruption sessions implicating Rovustatin were found to reverse the latency of HIV and inhibit the induction of gag protein-specific T-Lymphocyte responses in patients with AIDS (Hsieh et al., 1999). Hence, the novel coronavirus is able to infect helper CD4+ and cytotoxic CD8+ T-lymphocytes via the CXCR4 and CCR5 co-receptors (Agresti N. et al., 2021), and it may be able to directly impact their activity and even integrity. The human immunodeficiency retrovirus is capable of causing the same effects. Also, the unexpectedly high extent and diversity of damages caused by the virus and the spike glycoprotein strongly suggests there are unnatural origins of the virus that should be investigated with great care.
There are major similarities between SARS-CoV-2-induced COVID-19 and HIV-1-induced AIDS with regards to the principal mechanisms of innate immune activation and signaling as well. Namely, both viruses utilize genetic self-camouflaging methods to prevent a recognition of its pathogen-associated molecular patterns (PAMPs) by various Pattern Recognition Receptors (PRRs), Whilst SARS-CoV-2 mainly evades recognition by Toll-Like Receptors 3, 7 and 8 (TLR-3, 7 and 8), HIV-1 was shown to widely evade recognition by Toll-Like Receptors 8 (Campbell et al., 2021) and 9 (TLR-8 and 9) (Bernstein R. et al., 2017), and both viruses mimic several host cell proteins to evade first-line immunity. Once infecting macrophages, both single-stranded RNA viruses activate inflammasomes through a non-classical pathway, via the Guanine-Uracil-rich ssRNA. Researchers discovered that Pacrinitib inhibits IRAK-1 and reduces exaggerated TLR-8 signalling in both COVID-19 and AIDS (Campbell et al., 2017). Also, both viruses are known for their abilities to induce the phenomenon called autoholoimmunity, which was discovered by Root-Bernstein and which defines a set of immune responses that are both antimicrobial and anti-itself. Furthermore, a low dosage of the antimalarial quinine-derived compounds has shown efficacy as a mid-term to late therapy against both SARS-CoV-2 (Yu et al., 2020) and HIV-1, and in one study, it was shown to reduce the HIV-1 viral load in breast milk (LactMed, 2021), and low-dose Interferon I-based compounds have been indicated as prophylactic and early therapeutic agents for both diseases. Furthermore, it was discovered that quinacrine and chloroquine increased the antiviral effects of the 3’ - azido - 3’ - deoxythymidine drug in patients infected with HIV (Torres et al., 2015), although a high dosage of the two antimalarial drugs could be associated with increased risks of moderate and severe adverse events, which may involve digestive and cardiac symptoms, particularly in people with morbidity predispositions as such. It is interesting to note that a low dosage of Ivermectin has shown antiviral efficacy against SARS-CoV-2 (Kinobe et al., 2021) and HIV-1 (Waggstaff et al., 2012), although it is important to note that the antiviral effects of the drug are classed as broad-spectrum (Jans et al., 2020). For example, Ivermectin was shown to prevent the binding of the spike glycoprotein to the ACE2 receptor by docking on its receptor-binding domain, and it was also shown to specifically inhibit the nuclear import mediated by importin alpha/beta, leading to a decreased replication rate of HIV-1. Furthermore, twenty plant polyphenolic natural substances, including tannins and flavonoids, which are known to inhibit the activity of HIV Reverse Transcriptases were shown to have in-silico inhibitory activities against SARS-CoV-2 non-structural proteins 3, 5, 10, 12, 13, 15 and 16, which are known to inhibit the interferon system both indirectly and directly, and which ultimately play a major role in the induction of the COVID-19 disease (de Leon et al., 2021).
A wider phenomenon of HIV-1/LINE-1 Reverse Transcription of around 1% of the RNA nucleotides encoding the spike glycoprotein could significantly increase risks of induced mutation, mutagenesis and/or genome toxicity, particularly for people with a family history of cancer and immune diseases, as well as for people experiencing co-morbidities, having weaker DNA Repair Mechanisms or having a compromised immune system. Patients experiencing significant and widespread adverse reactions to the vaccine may also be more susceptible to such mutations, as the LNP-encapsulated nucleoside-modified mRNA would enter a higher number of cells and types of cells, thereby increasing the probability that it would enter cells containing proto-oncogenes or tumor-suppressor genes. It is known that large proportions of the population are susceptible to at least a form of cancer in their lifetime, and consequently, such molecular events could often result in a less restricted growth of tumorous tissues, which in turn often result in an increased risk of angiogenesis and metastasis. Such a phenomenon of HIV-1 Reverse Transcription is extremely rare in non-COVID-19 ribonucleic acid-based viruses, which can only increase suspicions that SARS-CoV-2 has unnatural origins, and even the manipulation of around 0.5% of the virus during a gain-of-function laboratory research could significantly change its nature and make it more dangerous for at least certain organs and systems of organs in the human body. A former MI5 British Intelligence employee once stated that it is virtually impossible to demonstrate that the virus was leaked from a gain-of-function laboratory environment due to the nature of the political regime in China.
Given that Type I and III Interferons very possibly have powerful prophylactic, immunizing and early therapeutic effects against both SARS-CoV-2 and HIV-1, it is possible that the innate, cellular and mucosal sectors of the human immune system contain important hidden powers against pathogenic viruses that have major abilities to self-camouflage and escape first-line immunity. It is possible that natural and mucosal immunity is the result of the majority of people infected with the novel coronavirus experiencing little to no symptoms of the disease, as they could be deemed as major natural barriers, preventing the viral load from reaching areas of the body where the effects of the disease are more powerful. It has been indicated that COVID-19 actually impacts the circulatory system the most, and not the respiratory tract, as previously projected (Salk Institute, 2021), and perhaps it is the significant targeting of the endothelial barrier by the virus and its main component of virulence, the spike protein, that supports this amendment of scientific projection. Likewise, if the novel coronavirus has a few, but major commonalities in infection and virulence with the human immunodeficiency virus, there may still be a major hope in the room; the possibility to catalyze natural and cellular immune processes before and during the first stages of the viral infection. Given that Type I and III Interferons simulate an event of cellular infection, products containing a low-dose of such cytokines may count as a vaccine candidate for both SARS-CoV-2-induced COVID-19 and HIV-1-induced AIDS (Carp T. et al., 2022). […]
It is important to note that a set of similarities represents a spectrum, rather than a yes-or-no question with regards to whether two microbes are genetically identical. And such a spectrum applies differently, depending on the context and background of the two genetic toxins to be compared. With regards to a genetic and phenotypic comparison between SARS-CoV-2 and HIV-1, it is important to apprehend that even a pronouncedly small degree of similarity could impact scientific and research perspective if such a level of similarity affects important areas in therapeutics and vaccinology, for example. Even if the two single-stranded ribonucleic acid-based viral agents are widely different from each other, if there is a genetic similarity in a few ribonucleic acid areas that are part of the viral genome impacting human immunity directly, then it is rather likely that the latter viral agent would also affect human immunity in similar patterns, which would affect the general approach of therapy and vaccine-development. Likewise, specific similarities between SARS-CoV-2 and HIV-1 with regards to induced immunopathogenesis does not ultimately indicate the coronavirus contains direct inserts from the retrovirus in cause, just as small-scale genetic and evolutionary similarities between the two viruses does not ultimately indicate a laboratory origin. In medical and biomedical research, it is likely crucial to hold fast to having an open mind and a humble approach in order not to become victims to the elementary, and yet still tricky, fallacy of “it is sunny, therefore it is not raining”. It is therefore a likelihood that the mechanisms and genetic origins of the novel coronavirus deserve further investigations to address found similarities in immunopathogenesis, genetics and proteomics that may be of significant concern, and to clarify genuine questions that numerous members of the public may be having, given that not every citizen and resident of the world has a degree in medicine or a biomedical science-related domain and that not all questions are in accordance with part or whole misinformation and with far-fetched conspiracy theories.”
I will research for more data to investigate similarities between the two viruses. I honestly believe this information needs to be on the table of all public health experts and that they need to be discussed transparently, live. The solution to the current problems is more powerful than many people currently believe, and there is still hope, although the required efforts to reverse much of the damage will be enormous. In short, it involves a reset of the immune system, comprising the administration of a low-dose derivatives of immunosuppressant antimalarial and antifungal drugs, quinine and ivermectin respectively, followed soon by the administration of a low-dose Interferon I and III-based compound to restart the immune system by re-sensitizing first-line immunity and making it faster than before. We need to stand up for the truth together so the experimental vaccines are halted immediately and that real medicine will take control and start repairing the unprecedented harms done by Big Pharma and its associates.
Featured image: By Photo Credit: C. GoldsmithContent Providers: CDC/ C. Goldsmith, P. Feorino, E. L. Palmer, W. R. McManus – This media comes from the Centers for Disease Control and Prevention’s Public Health Image Library (PHIL), with identification number #10000.Note: Not all PHIL images are public domain; be sure to check copyright status and credit authors and content providers.العربية | Deutsch | English | македонски | slovenščina | +/−, Public Domain, https://commons.wikimedia.org/w/index.php?curid=3909584
References:
Illanes-Álvarez, F., Márquez-Ruiz, D., Márquez-Coello, M., Cuesta-Sancho, S., & Girón-González, J. A. (2021). Similarities and differences between HIV and SARS-CoV-2. International journal of medical sciences, 18(3), 846–851. https://doi.org/10.7150/ijms.50133
Büttiker, P., Stefano, G. B., Weissenberger, S., Ptacek, R., Anders, M., Raboch, J., & Kream, R. M. (2022). HIV, HSV, SARS-CoV-2 and Ebola Share Long-Term Neuropsychiatric Sequelae. Neuropsychiatric disease and treatment, 18. , 2229–2237https://doi.org/10.2147/NDT.S382308
Riou, C., du Bruyn, E., Stek, C., Daroowala, R., Goliath, R. T., Abrahams, F., Said-Hartley, Q., Allwood, B. W., Hsiao, N. Y., Wilkinson, K. A., Arlehamn, C. S. L., Sette, A., Wasserman, S., Wilkinson, R. J., & HIATUS consortium (2021). Relationship of SARS-CoV-2-specific CD4 response to COVID-19 severity and impact of HIV-1 and tuberculosis coinfection. The Journal of clinical investigation, 131(12), e149125. https://doi.org/10.1172/JCI149125
Kim, E. H., Nguyen, T. Q., Casel, M. A. B., Rollon, R., Kim, S. M., Kim, Y. I., Yu, K. M., Jang, S. G., Yang, J., Poo, H., Jung, J. U., & Choi, Y. K. (2022). Coinfection with SARS-CoV-2 and Influenza A Virus Increases Disease Severity and Impairs Neutralizing Antibody and CD4+ T Cell Responses. Journal of virology, 96(6), e0187321. https://doi.org/10.1128/jvi.01873-21
Demoliou, C., Papaneophytou, C., & Nicolaidou, V. (2022). SARS-CoV-2 and HIV-1: So Different yet so Alike.Immune Response at the Cellular and Molecular Level. International journal of medical sciences, 19(12), 1787–1795. https://doi.org/10.7150/ijms.73134
Naidoo, N., Moodley, J., Khaliq, O. P., & Naicker, T. (2022). Neuropilin-1 in the pathogenesis of preeclampsia, HIV-1, and SARS-CoV-2 infection: A review. Virus research, 319, 198880. https://doi.org/10.1016/j.virusres.2022.198880
Witvrouwen, I., Mannaerts, D., Ratajczak, J., Boeren, E., Faes, E., Van Craenenbroeck, A. H., Jacquemyn, Y., & Van Craenenbroeck, E. M. (2021). MicroRNAs targeting VEGF are related to vascular dysfunction in preeclampsia. Bioscience reports, 41(8), BSR20210874. https://doi.org/10.1042/BSR20210874
Fischer, W., Giorgi, E. E., Chakraborty, S., Nguyen, K., Bhattacharya, T., Theiler, J., Goloboff, P. A., Yoon, H., Abfalterer, W., Foley, B. T., Tegally, H., San, J. E., de Oliveira, T., Network for Genomic Surveillance in South Africa (NGS-SA), Gnanakaran, S., & Korber, B. (2021). HIV-1 and SARS-CoV-2: Patterns in the evolution of two pandemic pathogens. Cell host & microbe, 29(7), 1093–1110. https://doi.org/10.1016/j.chom.2021.05.012
Azkur, A. K., Akdis, M., Azkur, D., Sokolowska, M., van de Veen, W., Brüggen, M. C., O'Mahony, L., Gao, Y., Nadeau, K., & Akdis, C. A. (2020). Immune response to SARS-CoV-2 and mechanisms of immunopathological changes in COVID-19. Allergy, 75(7), 1564–1581. https://doi.org/10.1111/all.14364
Wainberg M. A. (2004). HIV-1 subtype distribution and the problem of drug resistance. AIDS (London, England), 18 Suppl 3, S63–S68. https://doi.org/10.1097/00002030-200406003-00012
Abel, T., Moodley, J., Khaliq, O. P., & Naicker, T. (2022). Vascular Endothelial Growth Factor Receptor 2: Molecular Mechanism and Therapeutic Potential in Preeclampsia Comorbidity with Human Immunodeficiency Virus and Severe Acute Respiratory Syndrome Coronavirus 2 Infections. International journal of molecular sciences, 23(22), 13752. https://doi.org/10.3390/ijms232213752
Witvrouwen, I., Mannaerts, D., Ratajczak, J., Boeren, E., Faes, E., Van Craenenbroeck, A. H., Jacquemyn, Y., & Van Craenenbroeck, E. M. (2021). MicroRNAs targeting VEGF are related to vascular dysfunction in preeclampsia. Bioscience reports, 41(8), BSR20210874. https://doi.org/10.1042/BSR20210874
Tarasova, O., Ivanov, S., Filimonov, D. A., & Poroikov, V. (2020). Data and Text Mining Help Identify Key Proteins Involved in the Molecular Mechanisms Shared by SARS-CoV-2 and HIV-1. Molecules (Basel, Switzerland), 25(12), 2944. https://doi.org/10.3390/molecules25122944
Lesko, C. R., & Bengtson, A. M. (2021). HIV and COVID-19: Intersecting Epidemics With Many Unknowns. American journal of epidemiology, 190(1), 10–16. https://doi.org/10.1093/aje/kwaa158
Favara, G., Barchitta, M., Maugeri, A., Faro, G., & Agodi, A. (2022). HIV infection does not affect the risk of death of COVID-19 patients: A systematic review and meta-analysis of epidemiological studies. Journal of global health, 12, 05036. https://doi.org/10.7189/jogh.12.05036
Lee, K. W., Yap, S. F., Ngeow, Y. F., & Lye, M. S. (2021). COVID-19 in People Living with HIV: A Systematic Review and Meta-Analysis. International journal of environmental research and public health, 18(7), 3554. https://doi.org/10.3390/ijerph18073554
Gatechompol, S., Avihingsanon, A., Putcharoen, O., Ruxrungtham, K., & Kuritzkes, D. R. (2021). COVID-19 and HIV infection co-pandemics and their impact: a review of the literature. AIDS research and therapy, 18(1), 28. https://doi.org/10.1186/s12981-021-00335-1
Barbera, L. K., Kamis, K. F., Rowan, S. E., Davis, A. J., Shehata, S., Carlson, J. J., Johnson, S. C., & Erlandson, K. M. (2021). HIV and COVID-19: review of clinical course and outcomes. HIV research & clinical practice, 22(4), 102–118. https://doi.org/10.1080/25787489.2021.1975608
Sun, N., & Yau, S. S. (2022). In-depth investigation of the point mutation pattern of HIV-1. Frontiers in cellular and infection microbiology, 12. , 1033481https://doi.org/10.3389/fcimb.2022.1033481
Patel, R. H., Acharya, A., Chand, H. S., Mohan, M., & Byrareddy, S. N. (2021). Human Immunodeficiency Virus and Severe Acute Respiratory Syndrome Coronavirus 2 Coinfection: A Systematic Review of the Literature and Challenges. AIDS research and human retroviruses, 37(4), 266–282. https://doi.org/10.1089/AID.2020.0284
Tarcsai, K. R., Corolciuc, O., Tordai, A., & Ongrádi, J. (2022). SARS-CoV-2 infection in HIV-infected patients: potential role in the high mutational load of the Omicron variant emerging in South Africa. GeroScience, 44. (5), 2337–2345https://doi.org/10.1007/s11357-022-00603-6
Kuklina E. M. (2022). T Lymphocytes as Targets for SARS-CoV-2. Biochemistry. Biokhimiia, 87(6), 566–576. https://doi.org/10.1134/S0006297922060086
Shen, X. R., Geng, R., Li, Q., Chen, Y., Li, S. F., Wang, Q., Min, J., Yang, Y., Li, B., Jiang, R. D., Wang, X., Zheng, X. S., Zhu, Y., Jia, J. K., Yang, X. L., Liu, M. Q., Gong, Q. C., Zhang, Y. L., Guan, Z. Q., Li, H. L., … Zhou, P. (2022). ACE2-independent infection of T lymphocytes by SARS-CoV-2. Signal transduction and targeted therapy, 7(1), 83. https://doi.org/10.1038/s41392-022-00919-x
Sigalov A. B. (2022). SARS-CoV-2 may affect the immune response via direct inhibition of T cell receptor: Mechanistic hypothesis and rationale. Biochimie, 195, 86–89. https://doi.org/10.1016/j.biochi.2021.11.005
Garmendia, J. V., García, A. H., De Sanctis, C. V., Hajdúch, M., & De Sanctis, J. B. (2022). Autoimmunity and Immunodeficiency in Severe SARS-CoV-2 Infection and Prolonged COVID-19. Current issues in molecular biology, 45(1), 33–50. https://doi.org/10.3390/cimb45010003
Dotan, A., Muller, S., Kanduc, D., David, P., Halpert, G., & Shoenfeld, Y. (2021). The SARS-CoV-2 as an instrumental trigger of autoimmunity. Autoimmunity reviews, 20(4), 102792. https://doi.org/10.1016/j.autrev.2021.102792
Mobasheri, L., Nasirpour, M. H., Masoumi, E., Azarnaminy, A. F., Jafari, M., & Esmaeili, S. A. (2022). SARS-CoV-2 triggering autoimmune diseases. Cytokine, 154, 155873. https://doi.org/10.1016/j.cyto.2022.155873
Di Simone, M., Corsale, A. M., Lo Presti, E., Scichilone, N., Picone, C., Giannitrapani, L., Dieli, F., & Meraviglia, S. (2022). Phenotypical and Functional Alteration of γδ T Lymphocytes in COVID-19 Patients: Reversal by Statins. Cells, 11(21), 3449. https://doi.org/10.3390/cells11213449
Li, H., Chaudhry, S., Poonia, B., Shao, Y., & Pauza, C. D. (2013). Depletion and dysfunction of Vγ2Vδ2 T cells in HIV disease: mechanisms, impacts and therapeutic implications. Cellular & molecular immunology, 10(1), 42–49. https://doi.org/10.1038/cmi.2012.50
, A. A., Pollakis, G., Linnemann, T., Paxton, W. A., & de Baar, M. P. (2007). Statins disrupt CCR5 and RANTES expression levels in CD4(+) T lymphocytes in vitro and preferentially decrease infection of R5 versus X4 HIV-1. PloS one, 2(5), e470. https://doi.org/10.1371/journal.pone.0000470
, E. A., Jaimes, F. A., Rugeles, M. T., & Montoya, C. J. (2013). In vivo effect of statins on the expression of the HIV co-receptors CCR5 and CXCR4. AIDS research and therapy, 10, 10. https://doi.org/10.1186/1742-6405-10-10
Hsieh, S. M., Pan, S. C., Huang, Y. S., & Chang, S. C. (2021). Reversal of Viral Latency and Induction of Gag-Specific T-Cell Responses in HIV-1-Infected Adults Through Cyclic Treatment Interruption of Rosuvastatin: A Proof-of-Concept Study. Journal of acquired immune deficiency syndromes (1999), 86(4), 500–508. https://doi.org/10.1097/QAI.0000000000002577
Gilbert, C., Bergeron, M., Méthot, S., Giguère, J. F., & Tremblay, M. J. (2005). Statins could be used to control replication of some viruses, including HIV-1. Viral immunology, 18(3), 474–489. https://doi.org/10.1089/vim.2005.18.474
DaFonseca, S., Niessl, J., Pouvreau, S., Wacleche, V. S., Gosselin, A., Cleret-Buhot, A., Bernard, N., Tremblay, C., Jenabian, M. A., Routy, J. P., & Ancuta, P. (2015). Impaired Th17 polarization of phenotypically naive CD4(+) T-cells during chronic HIV-1 infection and potential restoration with early ART. Retrovirology, 12, 38. https://doi.org/10.1186/s12977-015-0164-6
Salwe, S., Padwal, V., Nagar, V., Patil, P., & Patel, V. (2019). T cell functionality in HIV-1, HIV-2 and dually infected individuals: correlates of disease progression and immune restoration. Clinical and experimental immunology, 198(2), 233–250. https://doi.org/10.1111/cei.13342
Allers, K., Puyskens, A., Epple, H. J., Schürmann, D., Hofmann, J., Moos, V., & Schneider, T. (2016). The effect of timing of antiretroviral therapy on CD4+ T-cell reconstitution in the intestine of HIV-infected patients. Mucosal immunology, 9(1), 265–274. https://doi.org/10.1038/mi.2015.58
Costiniuk, C. T., & Angel, J. B. (2012). Human immunodeficiency virus and the gastrointestinal immune system: does highly active antiretroviral therapy restore gut immunity?. Mucosal immunology, 5(6), 596–604. https://doi.org/10.1038/mi.2012.82
Nastri, B. M., Zannella, C., Folliero, V., Rinaldi, L., Restivo, L., Stelitano, D., Sperlongano, R., Adinolfi, L. E., & Franci, G. (2020). Editorial - Role of Highly Active Antiretroviral Therapy (HAART) for the COVID-19 treatment. European review for medical and pharmacological sciences, 24. https://doi.org/10.26355/eurrev_202011_23861(22), 11982–11984
Carp T, Metoudi M. Low-Dose Interferon I and III-Based Nasal Sprays: A Good-Looking COVID-19 Vaccine Candidate?. Preprints.org; 2022. DOI: 10.20944/preprints202212.0155.v2
Setaro, A. C., & Gaglia, M. M. (2021). All hands on deck: SARS-CoV-2 proteins that block early anti-viral interferon responses. Current research in virological science, 2, 100015. https://doi.org/10.1016/j.crviro.2021.100015
Rashid, F., Xie, Z., Suleman, M., Shah, A., Khan, S., & Luo, S. (2022). Roles and functions of SARS-CoV-2 proteins in host immune evasion. Frontiers in immunology, 13, 940756. https://doi.org/10.3389/fimmu.2022.940756
Zhang, L., Li, Q., Liang, Z., Li, T., Liu, S., Cui, Q., Nie, J., Wu, Q., Qu, X., Huang, W., & Wang, Y. (2022). The significant immune escape of pseudotyped SARS-CoV-2 variant Omicron. Emerging microbes & infections, 11(1), 1–5. https://doi.org/10.1080/22221751.2021.2017757
Raghavan, S., Kenchappa, D. B., & Leo, M. D. (2021, May 19). SARS-COV-2 spike protein induces degradation of junctional proteins that maintain endothelial barrier integrity. Frontiers. Retrieved December 5, 2022, from https://www.frontiersin.org/articles/10.3389/fcvm.2021.687783/full
Jafarzadeh, A., Chauhan, P., Saha, B., Jafarzadeh, S., & Nemati, M. (2020). Contribution of monocytes and macrophages to the local tissue inflammation and cytokine storm in COVID-19: Lessons from SARS and MERS, and potential therapeutic interventions. Life sciences, 257, 118102. https://doi.org/10.1016/j.lfs.2020.118102
Brown, M., & Bhardwaj, N. (2021). Super(antigen) target for SARS-CoV-2. Nature reviews. Immunology, 21(2), 72. https://doi.org/10.1038/s41577-021-00502-5
Huang, Y., Xie, J., Guo, Y., Sun, W., He, Y., Liu, K., Yan, J., Tao, A., & Zhong, N. (2021). SARS-CoV-2: Origin, Intermediate Host and Allergenicity Features and Hypotheses. Healthcare (Basel, Switzerland), 9(9), 1132. https://doi.org/10.3390/healthcare9091132
Grifoni, A., Weiskopf, D., Ramirez, S.I., Mateus, J., Dan, J.M., Moderbacher, C.R., Rawlings, S.A., Sutherland, A., Premkumar, L., Jadi, R.S., Marrama, D., de Silva, A.M., Frazier, A., Carlin, A.F., Greenbaum, J.A., Peters, B., Krammer, F., Smith, D.M., Crotty, S., & Sette, A. (2020). Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell, 181(7):1489-1501.e15. https://doi.org/10.1016/j.cell.2020.05.015
Mary Hongying Cheng, She Zhang, Rebecca A. Porritt, Magali Noval Rivas, Lisa Paschold, Edith Willscher, Mascha Binder, Mosche Arditi and Ivet Bahar (2020), Superantigenic character of an insert unique to SARS-CoV-2 spike supported by skewed TCR repertoire in patients with hyperinflammation, Proceedings of the National Academy of Sciences of the United States of America, 117(41, doi: ), pp 25254-25262https://doi.org/10.1073/pnas.2010722117
Bruttel, V., Washburne, A., & VanDongen, A. (2022). Endonuclease fingerprint indicates a synthetic origin of SARS-COV-2. https://doi.org/10.1101/2022.10.18.512756
Fleming, D.R.M. (2021). Is COVID-19 a Bioweapon?: A Scientific and Forensic investigation. Skyhorse Publishing (NY). ISBN 978-1-5107-7019-5
Lyons-Weiler, J. (2020). Pathogenic priming likely contributes to serious and critical illness and mortality in COVID-19 via autoimmunity. J Transl Autoim, 3: 100051. https://doi.org/10.1016/j.jtauto.2020.100051
Moser, D., Biere, K., Han, B., Hoerl, M., Schelling, G., Choukér, A., & Woehrle, T. (2021). COVID-19 Impairs Immune Response to Candida albicans. Frontiers in immunology, 12, 640644. https://doi.org/10.3389/fimmu.2021.640644
Yu, W., Wu, X., Zhao, Y., Chen, C., Yang, Z., Zhang, X., Ren, J., Wang, Y., Wu, C., Li, C., Chen, R., Wang, X., Zheng, W., Liao, H., & Yuan, X. (2021). Computational Simulation of HIV Protease Inhibitors to the Main Protease (Mpro) of SARS-CoV-2: Implications for COVID-19 Drugs Design. Molecules (Basel, Switzerland), 26(23), 7385. https://doi.org/10.3390/molecules26237385
Copertino, D. C., Jr, Casado Lima, B. C., Duarte, R. R. R., Powell, T. R., Ormsby, C. E., Wilkin, T., Gulick, R. M., de Mulder Rougvie, M., & Nixon, D. F. (2022). Antiretroviral drug activity and potential for pre-exposure prophylaxis against COVID-19 and HIV infection. Journal of biomolecular structure & dynamics, 40. (16), 7367–7380https://doi.org/10.1080/07391102.2021.1901144
Dallocchio, R. N., Dessì, A., De Vito, A., Delogu, G., Serra, P. A., & Madeddu, G. (2021). Early combination treatment with existing HIV antivirals: an effective treatment for COVID-19?. European review for medical and pharmacological sciences, 25. (5), 2435–2448https://doi.org/10.26355/eurrev_202103_25285
Magro, P., Zanella, I., Pescarolo, M., Castelli, F., & Quiros-Roldan, E. (2021). Lopinavir/ritonavir: Repurposing an old drug for HIV infection in COVID-19 treatment. Biomedical journal, 44(1), 43–53. https://doi.org/10.1016/j.bj.2020.11.005
Smolders, E. J., Te Brake, L. H., & Burger, D. M. (2020). SARS-CoV-2 and HIV protease inhibitors: why lopinavir/ritonavir will not work for COVID-19 infection. Antiviral therapy, 25(7), 345–347. https://doi.org/10.3851/IMP3365
Agarwal, S., & Agarwal, S. K. (2021). Lopinavir-Ritonavir in SARS-CoV-2 Infection and Drug-Drug Interactions with Cardioactive Medications. Cardiovascular drugs and therapy, 35(3), 427–440. https://doi.org/10.1007/s10557-020-07070-1
Agresti, N., Lalezari, J. P., Amodeo, P. P., Mody, K., Mosher, S. F., Seethamraju, H., Kelly, S. A., Pourhassan, N. Z., Sudduth, C. D., Bovinet, C., ElSharkawi, A. E., Patterson, B. K., Stephen, R., Sacha, J. B., Wu, H. L., Gross, S. A., & Dhody, K. (2021). Disruption of CCR5 signaling to treat COVID-19-associated cytokine storm: Case series of four critically ill patients treated with leronlimab. Journal of translational autoimmunity, 4, 100083. https://doi.org/10.1016/j.jtauto.2021.100083
de Leon, V.N.O., Manzano, J.A.H., Pilapil, D.Y.H. et al. Anti-HIV reverse transcriptase plant polyphenolic natural products with in silico inhibitory properties on seven non-structural proteins vital in SARS-CoV-2 pathogenesis. J Genet Eng Biotechnol 19, 104 (2021). https://doi.org/10.1186/s43141-021-00206-2
Knipping, F., Newby, G. A., Eide, C. R., McElroy, A. N., Nielsen, S. C., Smith, K., Fang, Y., Cornu, T. I., Costa, C., Gutierrez-Guerrero, A., Bingea, S. P., Feser, C. J., Steinbeck, B., Hippen, K. L., Blazar, B. R., McCaffrey, A., Mussolino, C., Verhoeyen, E., Tolar, J., Liu, D. R., … Osborn, M. J. (2022). Disruption of HIV-1 co-receptors CCR5 and CXCR4 in primary human T cells and hematopoietic stem and progenitor cells using base editing. Molecular therapy : the journal of the American Society of Gene Therapy, 30(1), 130–144. https://doi.org/10.1016/j.ymthe.2021.10.026
Guryanov, I., Real-Fernández, F., Sabatino, G., Prisco, N., Korzhikov-Vlakh, V., Biondi, B., Papini, A. M., Korzhikova-Vlakh, E., Rovero, P., & Tennikova, T. (2019). Modeling interaction between gp120 HIV protein and CCR5 receptor. Journal of peptide science : an official publication of the European Peptide Society, 25(2), e3142. https://doi.org/10.1002/psc.3142
Patterson, B. K., Seethamraju, H., Dhody, K., Corley, M. J., Kazempour, K., Lalezari, J. P., Pang, A. P., Sugai, C., Francisco, E. B., Pise, A., Rodrigues, H., Ryou, M., Wu, H. L., Webb, G. M., Park, B. S., Kelly, S., Pourhassan, N., Lelic, A., Kdouh, L., Herrera, M., … Sacha, J. B. (2020). Disruption of the CCL5/RANTES-CCR5 Pathway Restores Immune Homeostasis and Reduces Plasma Viral Load in Critical COVID-19. medRxiv : the preprint server for health sciences, 2020.05.02.20084673. https://doi.org/10.1101/2020.05.02.20084673
Blanpain, C., Libert, F., Vassart, G., & Parmentier, M. (2002). CCR5 and HIV infection. Receptors & channels, 8(1), 19–31.
Ribeiro, R. M., Hazenberg, M. D., Perelson, A. S., & Davenport, M. P. (2006). Naïve and memory cell turnover as drivers of CCR5-to-CXCR4 tropism switch in human immunodeficiency virus type 1: implications for therapy. Journal of virology, 80(2), 802–809. https://doi.org/10.1128/JVI.80.2.802-809.2006
Lambertini, A., Hartrampf, P. E., Higuchi, T., Serfling, S. E., Meybohm, P., Schirbel, A., Buck, A. K., & Werner, R. A. (2022). CXCR4-targeted molecular imaging after severe SARS-Cov-2 infection. European journal of nuclear medicine and molecular imaging, 50(1), 228–229. https://doi.org/10.1007/s00259-022-05932-4
Lourda, M., Dzidic, M., Hertwig, L., Bergsten, H., Palma Medina, L. M., Sinha, I., Kvedaraite, E., Chen, P., Muvva, J. R., Gorin, J. B., Cornillet, M., Emgård, J., Moll, K., García, M., Maleki, K. T., Klingström, J., Michaëlsson, J., Flodström-Tullberg, M., Brighenti, S., Buggert, M., … Karolinska KI/K COVID-19 Study Group (2021). High-dimensional profiling reveals phenotypic heterogeneity and disease-specific alterations of granulocytes in COVID-19. Proceedings of the National Academy of Sciences of the United States of America, 118(40), e2109123118. https://doi.org/10.1073/pnas.2109123118
Song, D., Adrover, J. M., Felice, C., Christensen, L. N., He, X. Y., Merrill, J. R., Wilkinson, J. E., Janowitz, T., Lyons, S. K., Egeblad, M., & Tonks, N. K. (2022). PTP1B inhibitors protect against acute lung injury and regulate CXCR4 signaling in neutrophils. JCI insight, 7(14), e158199. https://doi.org/10.1172/jci.insight.158199
Daoud, S., & Taha, M. (2022). Ligand-based Modeling of CXC Chemokine Receptor 4 and Identification of Inhibitors of Novel Chemotypes as Potential Leads towards New Anti- COVID-19 Treatments. Medicinal chemistry (Shariqah (United Arab Emirates)), 18(8), 871–883. https://doi.org/10.2174/1573406418666220118153541
Patterson, B. K., Seethamraju, H., Dhody, K., Corley, M. J., Kazempour, K., Lalezari, J., Pang, A. P. S., Sugai, C., Mahyari, E., Francisco, E. B., Pise, A., Rodrigues, H., Wu, H. L., Webb, G. M., Park, B. S., Kelly, S., Pourhassan, N., Lelic, A., Kdouh, L., Herrera, M., … Sacha, J. B. (2021). CCR5 inhibition in critical COVID-19 patients decreases inflammatory cytokines, increases CD8 T-cells, and decreases SARS-CoV2 RNA in plasma by day 14. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases, 103, 25–32. https://doi.org/10.1016/j.ijid.2020.10.101
Elneil, S., Lalezari, J. P., & Pourhassan, N. Z. (2021). Case study of a critically ill person with COVID-19 on ECMO successfully treated with leronlimab. Journal of translational autoimmunity, 4, 100097. https://doi.org/10.1016/j.jtauto.2021.100097
Tan, Q., Zhu, Y., Li, J., Chen, Z., Han, G. W., Kufareva, I., Li, T., Ma, L., Fenalti, G., Li, J., Zhang, W., Xie, X., Yang, H., Jiang, H., Cherezov, V., Liu, H., Stevens, R. C., Zhao, Q., & Wu, B. (2013). Structure of the CCR5 chemokine receptor-HIV entry inhibitor maraviroc complex. Science (New York, N.Y.), 341(6152), 1387–1390. https://doi.org/10.1126/science.1241475
Basha, G. M., Parulekar, R. S., Al-Sehemi, A. G., Pannipara, M., Siddaiah, V., Kumari, S., Choudhari, P. B., & Tamboli, Y. (2022). Design and in silicoinvestigation of novel Maraviroc analogues as dual inhibition of CCR-5/SARS-CoV-2 Mpro. Journal of biomolecular structure & dynamics, 40. (21), 11095–11110https://doi.org/10.1080/07391102.2021.1955742
Ancy, I., Sivanandam, M., & Kumaradhas, P. (2021). Possibility of HIV-1 protease inhibitors-clinical trial drugs as repurposed drugs for SARS-CoV-2 main protease: a molecular docking, molecular dynamics and binding free energy simulation study. Journal of biomolecular structure & dynamics, 39. (15), 5368–5375https://doi.org/10.1080/07391102.2020.1786459
Root-Bernstein R. Human Immunodeficiency Virus Proteins Mimic Human T Cell Receptors Inducing Cross-Reactive Antibodies. International Journal of Molecular Sciences. 2017; 18(10):2091. https://doi.org/10.3390/ijms18102091
Campbell, G. R., To, R. K., Hanna, J., & Spector, S. A. (2021). SARS-CoV-2, SARS-CoV-1, and HIV-1 derived ssRNA sequences activate the NLRP3 inflammasome in human macrophages through a non-classical pathway. iScience, 24(4), 102295. https://doi.org/10.1016/j.isci.2021.102295
Campbell, G. R., Rawat, P., & Spector, S. A. (2022). Pacritinib Inhibition of IRAK1 Blocks Aberrant TLR8 Signalling by SARS-CoV-2 and HIV-1-Derived RNA. Journal of innate immunity, 1–11. Advance online publication. https://doi.org/10.1159/000525292
Abramczyk, H., Brozek-Pluska, B., & Beton, K. (2022). Decoding COVID-19 mRNA Vaccine Immunometabolism in Central Nervous System: human brain normal glial and glioma cells by Raman imaging. bioRxiv.
Martinez, G. P., Zabaleta, M. E., Di Giulio, C., Charris, J. E., & Mijares, M. R. (2020). The Role of Chloroquine and Hydroxychloroquine in Immune Regulation and Diseases. Current pharmaceutical design, 26. https://doi.org/10.2174/1381612826666200707132920(35), 4467–4485
Yu, B., Li, C., Chen, P., Zhou, N., Wang, L., Li, J., Jiang, H., & Wang, D. W. (2020). Low dose of hydroxychloroquine reduces fatality of critically ill patients with COVID-19. Science China. Life sciences, 63(10), 1515–1521. https://doi.org/10.1007/s11427-020-1732-2
Lagier, J. C., Million, M., Gautret, P., Colson, P., Cortaredona, S., Giraud-Gatineau, A., Honoré, S., Gaubert, J. Y., Fournier, P. E., Tissot-Dupont, H., Chabrière, E., Stein, A., Deharo, J. C., Fenollar, F., Rolain, J. M., Obadia, Y., Jacquier, A., La Scola, B., Brouqui, P., Drancourt, M., … IHU COVID-19 Task force (2020). Outcomes of 3,737 COVID-19 patients treated with hydroxychloroquine/azithromycin and other regimens in Marseille, France: A retrospective analysis. Travel medicine and infectious disease, 36, 101791. https://doi.org/10.1016/j.tmaid.2020.101791
Torres, K. J., Reyes-Terán, G., Sotelo, J., Jung-Cook, H., & Aguirre-Cruz, L. (2015). Influence of quinacrine and chloroquine on the in vitro 3'-azido-3'-deoxythymidine antiretroviral effect. AIDS research and therapy, 12, 7. https://doi.org/10.1186/s12981-015-0048-9
Lehrer, S., & Rheinstein, P. H. (2020). Ivermectin Docks to the SARS-CoV-2 Spike Receptor-binding Domain Attached to ACE2. In vivo (Athens, Greece), 34. (5), 3023–3026https://doi.org/10.21873/invivo.12134
Kinobe, R. T., & Owens, L. (2021). A systematic review of experimental evidence for antiviral effects of ivermectin and an in silico analysis of ivermectin's possible mode of action against SARS-CoV-2. Fundamental & clinical pharmacology, 35(2), 260–276. https://doi.org/10.1111/fcp.12644
Jans, D. A., & Wagstaff, K. M. (2020). Ivermectin as a Broad-Spectrum Host-Directed Antiviral: The Real Deal?. Cells, 9(9), 2100. https://doi.org/10.3390/cells9092100
Wagstaff, K. M., Sivakumaran, H., Heaton, S. M., Harrich, D., & Jans, D. A. (2012). Ivermectin is a specific inhibitor of importin α/β-mediated nuclear import able to inhibit replication of HIV-1 and dengue virus. The Biochemical journal, 443(3), 851–856. https://doi.org/10.1042/BJ20120150
Zhang, L., Richards, A., Khalil, A., Wogram, E., Ma, H., Young, R. A., & Jaenisch, R. (2020). SARS-CoV-2 RNA reverse-transcribed and integrated into the human genome. bioRxiv : the preprint server for biology, 2020.12.12.422516. https://doi.org/10.1101/2020.12.12.422516
Aldén M, Olofsson Falla F, Yang D, Barghouth M, Luan C, Rasmussen M, De Marinis Y. Intracellular Reverse Transcription of Pfizer BioNTech COVID-19 mRNA Vaccine BNT162b2 In Vitro in Human Liver Cell Line. Current Issues in Molecular Biology. 2022; 44(3):1115-1126. https://www.mdpi.com/1467-3045/44/3/73/htm
Luisetto, M., Almukthar, N., & Tarro, G., Intracellular Reverse Transcription of COVID-19 mRNA Vaccine, LAP LAMBERT Academic Publishing. 2022; 1, 3-67. ISBN: 978-620-0-31572-4
Fertig TE, Chitoiu L, Marta DS, Ionescu V-S, Cismasiu VB, Radu E, Angheluta G, Dobre M, Serbanescu A, Hinescu ME, Gherghiceanu M. Vaccine mRNA Can Be Detected in Blood at 15 Days Post-Vaccination. Biomedicines. 2022; 10(7):1538. https://doi.org/10.3390/biomedicines10071538
Rodríguez, Y., Rojas, M., Beltrán, S., Polo, F., Camacho-Domínguez, L., Morales, S. D., Gershwin, M. E., & Anaya, J. M. (2022). Autoimmune and autoinflammatory conditions after COVID-19 vaccination. New case reports and updated literature review. Journal of autoimmunity, 132, 102898. https://doi.org/10.1016/j.jaut.2022.102898
Leone, M. C., Canovi, S., Pilia, A., Casali, A., Depietri, L., Fasano, T., Colla, R., & Ghirarduzzi, A. (2022). Four cases of acquired hemophilia A following immunization with mRNA BNT162b2 SARS-CoV-2 vaccine. Thrombosis research, 211, 60–62. https://doi.org/10.1016/j.thromres.2022.01.017
Chiu, S. N., Chen, Y. S., Hsu, C. C., Hua, Y. C., Tseng, W. C., Lu, C. W., Lin, M. T., Chen, C. A., Wu, M. H., Chen, Y. T., Chien, T. H., Tseng, C. L., & Wang, J. K. (2023). Changes of ECG parameters after BNT162b2 vaccine in the senior high school students. European journal of pediatrics, 1–8. Advance online publication. https://doi.org/10.1007/s00431-022-04786-0
[Retracted, but may be important for investigation] Pradhan P, Pandey AK, Mishra A, et al. Uncanny similarity of unique inserts in the 2019-nCoV spike protein to HIV-1 gp120 and Gag. bioRxiv; 2020. https://doi.org/10.1101/2020.01.30.927871.